Abstract
Background:
Post-transplant lymphoproliferative disease (PTLD) is a rare, but well-known complication of solid organ transplants and hematopoietic stem cell transplantation. . In most affected patients, PTLD is an Epstein-Barr virus (EBV)-positive B cell proliferation occurring in the setting of immunosuppression and decreased T cell immune surveillance. PTLDs are among the most serious complications of transplantation. The principal risk factors underlying the development of PTLD are the degree of T cell immunosuppression and the Epstein-Barr virus (EBV) serologic status of the recipient. Early lesions of PTLD are treated with reduction in immunosuppression alone and those who do not have a complete response to this intervention have been treated with chemotherapy, immunotherapy, and occasionally surgical resection. Utilizing the NCDB, we aim to study the clinical and demographic characteristics of PTLD patients who were declared dead during period of 2010-2017.
Methods
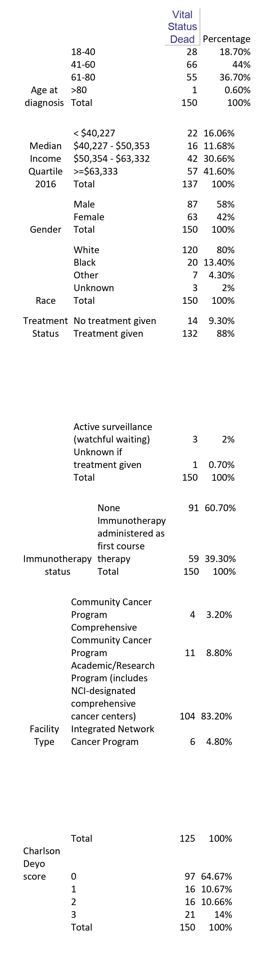
A total of 425 patients diagnosed with PTLD above the age of 18 years between 2010 and 2017 were identified utilizing the National Cancer Database (NCDB). Patients were identified with ICD-O-3 morphologic code 9971/3 and data extracted from PUF using SPSS. Demographic factors (Race, gender, facility location, annual household income, facility type, Charlson-Deyo score, treatment received, age at diagnosis) were studied in relation to patient's vital status (alive or dead). We have separated data for patients declared dead during this period and formulated a table stating the demographic characteristics. We have excluded people whose vital status was unknown or missing (60 patients).
Results
Of the 365 patients diagnosed with PTLD between 2010-2017, 215 patients were alive during the entire period and 150 (41%) were declared dead in this time frame. Of these, 62.7% were in the age group less than 60 years and 37.3% above 60 years. 9.3% (14/150) received no treatment at all and 88% received some form of treatment, of which 39.3% (59/150) received immunotherapy (34 received immunotherapy alone and 23 received Immuno+chemo). Amongst these, 80% were Caucasians and 13.4% were African Americans. 41.6% (57/137) belonged to median income quartile >=$63,333, whereas 16% (22/137) belonged to median quartile income <$40,227 (Median Quartiles 2012-2016). 83.2% received care at an academic/research program and 8.8% in a Comprehensive community cancer program. 64.7% (97/150) of patient's had Charlson-Deyo score of 0 whereas 14% (21/150) had a score of 3.
Conclusion
This study contains largest cohort of patients diagnosed with PTLD, identifying clinical and demographic factors of patients with PTLD who were declared dead during the period of 2010-2017. The data shows significant variations in the populations stratified based on age, income quartiles, treatment received and race. These data may provide insight into identifying the factors influencing mortality of patients diagnosed with PTLD. The major limitations of our study include no data on specific therapy received, reasons for choosing the treatment modality used, no data on the cause of mortality and age at death.
No relevant conflicts of interest to declare.